Sheffield patient shows immediate improvement after IR team performs mechanical thrombectomy to remove clots
Helen Foster of Hackenthorpe is one of the first patients in South Yorkshire to benefit from a treatment to remove clots from the blood vessels in her lungs. Mechanical thrombectomy uses a novel medical device to physically suck blood clots out from the lung.
Foster started to struggle with breathlessness and mobility problems a few weeks prior to her procedure but put it down to bad seizures. Things became worse and one evening she began to feel very unwell with dizziness, passing out and pain in her lower leg.
She was rushed to Northern General Hospital, part of Sheffield Teaching Hospitals NHS Foundation Trust. Given the severity of her embolism, Foster was offered the pioneering x-ray-guided treatment, which involves using image-guided technology and a mechanical device with a tiny suction cap attached to it to remove or dissolve large clots from the lungs.
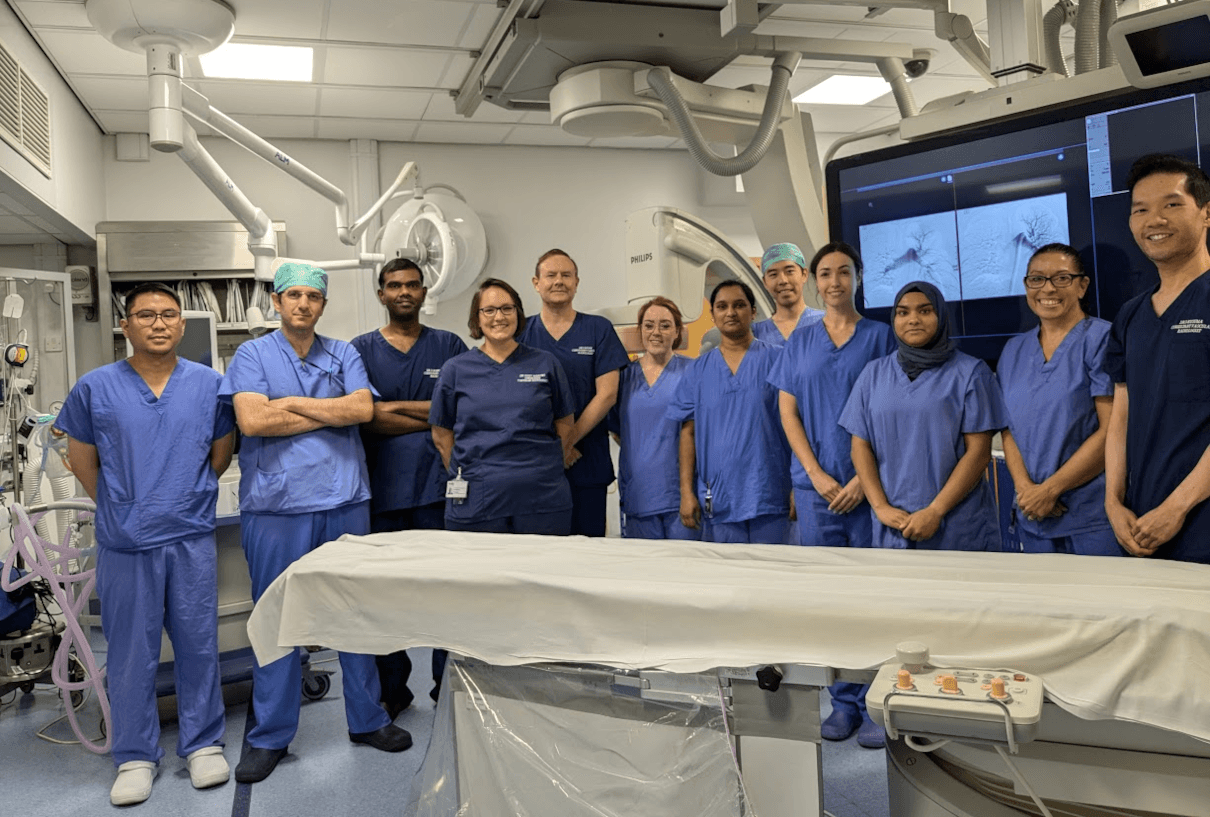
Performed by a team of radiologists with support from respiratory doctors and staff from the cardiac care unit, mechanical thrombectomy is carried out under local anaesthetic and normally lasts about an hour.
To access the veins, vascular interventional radiologists make a tiny incision into the groin. Using a catheter and guided by live low dose x-rays, the device is then pushed through the heart and into the blood vessels of the lungs. Once the pulmonary artery is reached, the mechanical device is deployed. For Foster, the benefits could be felt in minutes, with the team saying she visibly improved moments after the clots had been removed.
“It was absolutely unreal,” said Foster. “My chest was killing, and I felt like I was going to have a heart attack, but the pressure and pain in my lung just went as they cleared one side of the clot. When they did the other side, it was like ‘whoosh’, the pain in my heart was released and my breath had come back to almost normal.”
Consultant vascular and interventional radiologist Dr Dan Kusuma said: “The procedure involves close collaboration between several medical disciplines including respiratory care, cardiology, intensive care and interventional radiology. The outcomes have been quite remarkable, with patients who were quite unwell when they were referred to us improving significantly – and even visibly on the operating table – to the extent that they were able to be discharged home within one to two days.”
Picture: Consultant vascular and interventional radiologist Dr Dan Kusuma (right) and the team that performed the procedure on Helen Foster. Images from the procedure can be seen on the screen.
Published on page 22 of the October 2024 issue of RAD Magazine.